Corneal Edema
Last reviewed by Dr. Raj MD on January 12th, 2022.
What is Corneal Edema?
All over the world, there are millions of people who are operated upon for cataract. Unfortunately, like any other surgical intervention, the cataract surgery can lead to a number of complications. One of the most common complications is represented by the corneal edema. In the medical literature, this is also presented as bullous keratopathy (pseudophakic or aphakic). In the initial phase, the inflammatory process occurs in the stroma. Given the fact that this is a progressive condition, in a short period of time, the inflammation reaches the intercellular epithelial layer. The appearance of bullae is a sign that the inflammation or edema has gotten worse.

The number of people who have suffered from such complications has reduced in the past few years, thanks to the development of surgical methods and also to the innovative lens design. However, it should be mentioned that the corneal edema remains an often-encountered complication of cataract surgery. The highest risk is of visual disability, no matter if the procedure went according to the routine or there were any other complications associated to it.
Pathophysiology
The cornea can be defined as the transparent membrane that covers the eye (and more specifically the iris and the pupil, plus the anterior chamber). It is important to understand that, as long as the cornea remains dehydrated, the corneal transparency is going to be maintained. The presence of fluid in the cornea is suggestive of increased intraocular pressure. It can also be a sign of metabolic changes at the level of the epithelium. The loss of epithelium in the cornea can be caused not only by an inflammatory process but appear as well because of a surgical intervention (trauma) or as the direct result of corneal dystrophy.
Epidemiology
Despite the extensive studies made in the field, the exact incidence of the corneal edema has yet to be determined. Of all the complications that occur after the surgical intervention for cataract, the corneal edema accounts for 0.1%. Other statistics present the corneal edema as one of the major reasons for a corneal transplant. In regard to the gender or race predilection, no such predilections have been identified when it comes to corneal edema. In regard to the age, the elderly population is often affected by such problems (endothelium aging and associated loss).
Corneal Edema Signs and Symptoms
As the transparency of the cornea is reduced, the patient starts to suffer from impaired vision. The severity of the visual disability is in direct proportion to the intensity and progression of the corneal edema. As both the central and peripheral cornea suffer from a thickening process, the patient might experience pain in the affected eye and see a halo around the different sources of light. The foreign body sensation might appear, followed by the increased sensitivity to light (photophobia).
Because of the initial edema affecting the stroma, it is possible that the normal tear film is going to be disrupted. When vesicles or bullae are noticed on the surface of the cornea, this is suggestive of the fact that condition has reached an advanced stage. The patient will experience pain and photophobia, both symptoms becoming more intense as more bullae form and rupture at the level of the cornea. In patients who suffer from Fuchs dystrophy, it is possible to see cornea guttata, which is characterized by lesions at the level of the endothelium and a specific appearance (beaten metal).
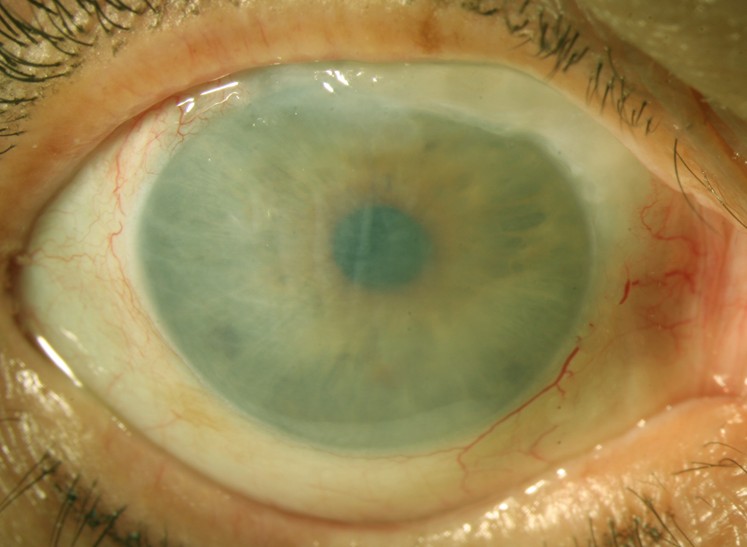
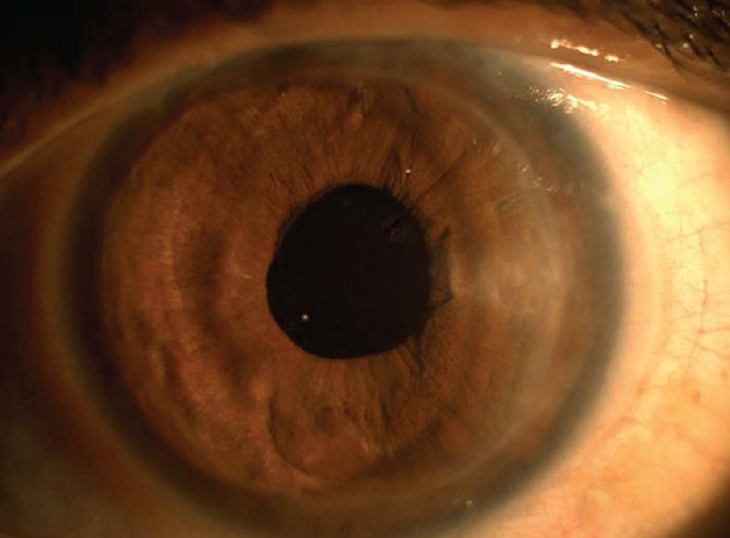
Pictures of Corneal Edema
Causes of Corneal Edema
These are the most common causes that can lead to the appearance of the corneal edema:
- Congenital hereditary endothelial dystrophy – form of corneal dystrophy diagnosed in the neonatal period and present at birth
- Schlichting dystrophy (posterior polymorphous corneal dystrophy) – form of corneal dystrophy, in which specific changes occurs at the level of the endothelium and in Descemet’s membranes
- Chandler’s syndrome (iridocorneal endothelial syndrome) – rare eye disorder, characterized by the proliferation of the endothelium and the distortion of the iris
- Acute narrow-angle glaucoma – medical condition, characterized by increased intraocular pressure (high risk of vision loss)
- Herpes simplex keratitis – medical condition, characterized by the inflammation of the cornea, due to the infection with the herpes simplex virus
- Corneal transplant rejection – as the eye rejects the newly-transplanted cornea, an inflammatory process occurs (edema)
- Surgical trauma (cataract surgery) – the cornea edema appears as a complication of cataract surgery. The risk for such complications is increased in patients who are also suffering from diabetes, due to the associated endothelial loss. In regard to the actual surgical intervention, the damage to the cornea is correlated with a number of factors, including the size and location of the incision. The density of the nucleus, the intensity of the ultrasound energy and the fluid quantity irrigating the eye are the other factors that can increase the risk of surgical trauma. The chosen surgical technique plays its part, leading to more or less endothelial cell loss. Touching the epithelium during the surgical intervention is one of the biggest mistakes that can be made. More recently, viscoelastic agents have started to be used in such surgical interventions, so as to reduce the potential endothelial cell loss and protect the cornea from trauma.
- Intraocular lenses (less modern versions) – increase the risk of endothelial cell loss after the cataract surgery. This is often seen in patients who are wearing closed-loop anterior chamber intraocular lenses, the endothelial cell loss being found in association with the chronic inflammatory process (low-grade).
- Fuchs dystrophy – this form of endothelial dystrophy is characterized by the presence of cornea guttata, which are produced at the level of the endothelium. This condition is more often diagnosed in women than men. It is also common in the older population.
- Inflammatory conditions of the eye (such as iritis or uveitis) – these contribute to the endothelial cell loss, which in turn leads to corneal edema
- Increased intraocular pressure (without glaucoma) – this condition leads to the appearance of fluid in the cornea, which triggers the acute onset of corneal edema
- Touching the vitreous and the anterior chamber – contributes to the endothelial cell loss, increasing the risk for corneal edema.
Diagnosis
Imaging studies are essential for the diagnosis of the corneal edema. Specular microscopy is one of the most recommended investigations, the photographic method allowing for the highly-efficient assessment of the endothelium. Thanks to the high-quality photographs of the endothelial layer that are taken, it is possible to assess the current density. In the situation that the cell density is under 1000 cells/mm2, there is a high risk of corneal edema. When analyzing the cells of the endothelial layer, the specialists are also looking at their size and shape. The more variable these are, the higher the risk of corneal edema. Specular microscopy can also be used to assess how much the corneal edema has progressed (in accordance to the endothelial loss).
Pachymetry (optical or ultrasound) is another method recommended for the diagnosis of the corneal edema. This method can be used in order to assess the thickness of the cornea. It is a known fact that, in patients diagnosed with this condition, the cornea thickens because of the inflammatory process. The suspicion of corneal edema is raised in the situation that the thickness of the cornea is over 0.6 mm. It is recommended that the thickness of the cornea is measured at different intervals, so as to assess the progression of the condition. While ultrasound pachymetry is sometimes preferred because it requires less skill, the optical pachymetry is chosen for the assessment of corneal scars or lesions.
The suspicion of corneal edema can be confirmed through histologic analysis as well. This can confirm the endothelial cell loss, identifying other characteristic changes (corneal guttata in patients with Fuchs dystrophy). It can also be used to identify the thickening at the level of the Descemet membrane.
Treatment
The main purpose of the treatment is to minimize the corneal edema, which in turn will improve the symptoms experienced by the patient, such as the visual disability, pain or discomfort. Hypertonic agents are generally recommended for the mild corneal edema; doctors often prescribe sodium chloride, under the form of solution or ointment, with the purpose of creating a hypertonic tear film (this will draw the water out of the cornea). Eye drops can be used in order to improve the quality of the vision.
Bandage contact lenses are used as adjuvants to the current medical treatment(s). These guarantee temporary relief from the pain or discomfort caused by the corneal edema, being treated with antibiotic substances (prevention of secondary bacterial infection). In the situation that the patients suffers from extremely intense pain, associated with visual disability, the anterior stromal puncture is preferred as a method of intervention.
In order for the epithelium to adhere to the underlying cornea, the excimer laser phototherapeutic keratectomy is used as a method of intervention. Severe cases benefit from corneal transplant, especially if there is vision loss and significant pain. The newest intervention of this form is known as the Descemet membrane endothelial keratoplasty. Other treatments recommended for the corneal edema include: antibiotic drops, prednisolone, brimonidine and timolol ophthalmic.
Prognosis
The prognosis of corneal edema is good in the majority of cases, especially in patients who have undergone a corneal transplant. However, the level of vision required for certain activities, such as reading or writing, is present in only half of the patients.